What to Do Now, So Your Bones Won't Be Frail Later
By Deborah Copaken
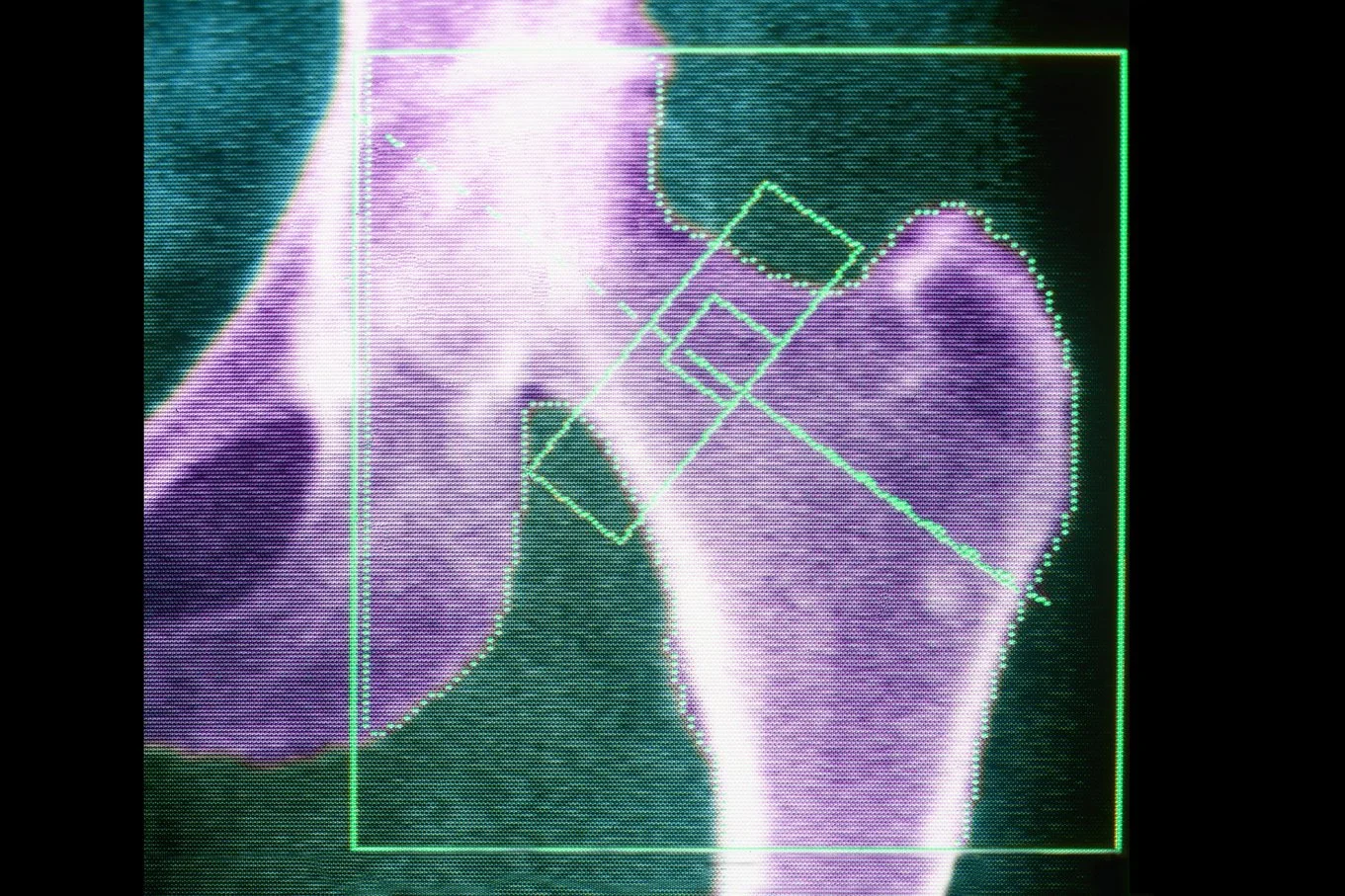
I had my first DEXA scan this past June, after both my primary care physician and my gynecologist suggested I get one. DEXA stands for dual x-ray absorptiometry, and I’m embarrassed to say I’d never heard of this test or its acronym until my conversation with Midi Health CEO Joanna Strober last October. DEXA scans measure bone density, which is the thickness and strength of our bones.
If you were born after 1958 and have never heard of a DEXA scan either, don’t be too hard on yourself. You’re not yet due for one unless you have certain risk factors for osteoporosis. The CDC lists intestinal disorders, multiple sclerosis, and low BMI, none of which I have. In fact, the CDC doesn’t even list surgical or early menopause — which I do have — as risk factors. Even though they most definitely are. And their guidelines don’t recommend getting a DEXA scan until age 65, if you are a woman, or 70, if you are a man.
I am 57. Too young, I thought, for osteoporosis. Well, guess what, kids? I was wrong. And my doctors were right to have me tested early. I wasn’t sure where to begin, now that I’d learned that I have the spine of an octogenarian and the hips of a woman in her seventies. Should I call an orthopedist? A spine specialist? What, exactly, was I dealing with here beyond the normal decay of age, and how does one go about rebuilding human bone?
Both my doctors suggested I consult with an endocrinologist. Finding one who takes my insurance was one thing. Getting an appointment with her was another. I was able to nab an appointment (checks notes) six months later, in December of 2023. But what to do with this diagnosis in the meantime? What should I be doing, taking? Is bone loss reversible? I wanted more information than I could glean from a simple Google search.
Then I remembered speaking with Dr. Mary O’Connor, an orthopedic surgeon and the co-author of Taking Care of You: The Empowered Woman's Guide to Better Health.
Turns out, my assumptions about osteoporosis being an old lady’s disease were incorrect. Nearly 1 in 5 women and 1 in 20 men over the age of fifty — fifty! — have osteoporosis. Simply put, this means we are at greater risk of breaking bones. Luckily, there are a few things we can do earlier in life to safeguard against this.
*Please note the conversation below has been adapted for Gloria readers.
Deborah Copaken: Had I been put on hormone therapy right after having my uterus removed, could I have avoided this?
Dr. Mary O'Connor: Most likely, yeah.You would've either avoided it or mitigated it. It wouldn't be as bad as it is now, because estrogen helps protect our bones.
Deborah Copaken: What does it mean to have osteoporosis? Let's just define our terms.
Dr. Mary O'Connor: Osteoporosis is basically when our bones have become weaker. That puts you at higher risk of a fracture. As we get older, fractures can be devastating. This is very, very important for women because post-menopause, we lose bone density at a higher rate. When we're young and we're growing, we're building bone. Our bones are growing not just in length and circumference, but in strength. We reach peak bone strength in our early 20s. The bad news is, [it’s] downhill from there.
Deborah Copaken: I've heard about maintaining bone health all my life. I'm healthy. I do yoga. I walk every single day. I eat yogurt and milk, all my leafy greens, and I still got osteoporosis?
Dr. Mary O'Connor: Sometimes we're just dealt the genetic osteoporosis card. And there's nothing you can do about that, except stay on top of it. What's important is that throughout our lifetimes we work on keeping healthy bones, and the key to all of that is weight-bearing exercises.
Deborah Copaken: What is a weight-bearing exercise?
Dr. Mary O'Connor: Weight-bearing exercises are running. Walking is a weight-bearing exercise, lifting weights, getting in the gym, and doing resistance exercises in the gym, because bones respond to stress. If you are exercising and putting more stress on the bones, the bones get stronger.
Deborah Copaken: I could be doing more weightlifting. Wouldn't yoga be considered the same as lifting weights?
Dr. Mary O'Connor: No, because it's not putting as much stress on your bones as if you were running, where you're pounding on the pavement, or you're doing weights. It's weight-bearing exercises, adequate calcium, and adequate vitamin D. This is where a lot of people have an opportunity to improve. Let's talk for a minute about vitamin D, because it's really, really important.
Vitamin D is actually a hormone. It has receptors in our body all over the place, including our muscle. If you give older patients more vitamin D and get their vitamin D levels up, they're less likely to fall. Vitamin D is also critically important to bone health, because if you don't have adequate vitamin D, you cannot absorb the calcium you eat.
Deborah Copaken: Okay, so what do I do to get vitamin D?
Dr. Mary O'Connor: Go to the vitamin shop and get vitamin D3. D3 is the best supplement form. Just buy a bottle that has 1,000 international units of vitamin D. They'll come in little gel caps, so they're very easy to swallow, and you just take one a day. It's hard to take too much vitamin D. Now, you should also make sure that your primary care doctor is checking your vitamin D level. A lot of them will do that now.
The three things that anyone can do right now [are]: weight-bearing exercises, adequate calcium, and adequate vitamin D. It's vitamin D that is such a huge opportunity, because when you look at studies, there are so many people that are low on vitamin D.
Deborah Copaken: All right. So now that I have osteoporosis, what are my options? Somebody told me about Prolia and Fosomax. What would you suggest?
Dr. Mary O'Connor: The frontline medications are called bisphosphonates, and there are several of them on the market, like Fosamax, Actonel, Boniva. Many of these pills can cause heartburn, upset stomach, some things like that. There's also an infusion. You can get the medicine into your veins. Now, I'll be a little bit controversial here.
Deborah Copaken: Be controversial. We love controversy here.
Dr. Mary O'Connor: We think of bone as being this inert substance. That is not true. Bone is living tissue. Bone is alive. Bone is constantly going through a process of resorption, meaning bone is eaten away and rebuilding, meaning bone is added. When we're young and growing, the building is greater than the resorption. When we get older, the resorption is greater than the rebuilding. That's why our bones get weaker. The bisphosphonates medications that are the frontline medical therapy block resorption of bone, so the bone doesn't get as weak.
One of the challenges with that is that in some cases — it's not common — think of the bone as almost getting frozen. It's like you've uncoupled the resorption and the rebuilding, and the bone becomes more inert, so to speak, and can fracture. And then those fractures are difficult to heal. When patients are put on these medications, it will be recommended frequently that, after a certain number of years, they have a drug holiday. You go off the medicine to give your bone a chance to go back to a more normal cycle. Now, there are other medications that work on stimulating the formation of bone, and so they work the exact opposite. Instead of saying, "Okay, we're going to keep your bones stronger by blocking the resorption," it's, "We're going to keep your bones stronger by stimulating more formation of bone." To me, that makes so much more sense.
Deborah Copaken: I thought I was taking care of my bone health, but I didn't know how vitamin D worked.
Dr. Mary O'Connor: We think of osteoporosis as a woman's disease, because it affects women more predominantly, but if you look at populations, we're not alone in this. Men get osteoporosis as well. Everybody in the family needs to be paying attention to bone health, not just women, but it affects us at an earlier age. We lose our bone density faster. Men also typically start off with a higher bone density strength as a young adult than a young woman, a girl, which is another reason why sports for girls are so important.
Deborah Copaken: I just didn't know that I wasn't taking care of myself, and suddenly here I am with osteoporosis.
Dr. Mary O'Connor: I'll close with this comment that I think is really important for us to remember. Osteoporosis is the silent killer, because what happens is, we break bones and the consequences of those fractures start us in that downward death spiral. We're all going to go some day, but we want to have a high quality of life up until the end, and that means not breaking your hip and not getting compression fractures in your spine, which cause chronic pain.